Explanation of lymphedema and cellulitis
Treatment of cellulitis, and suppression of onset by lymphatic venous anastomosis
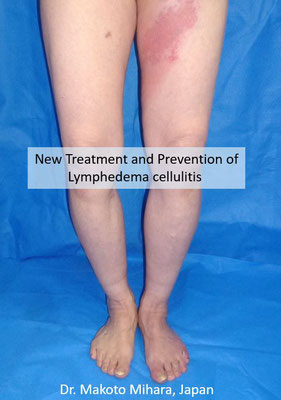
Lymphedema and cellulitis
It is thought that about 30% of lymphedema patients develop cellulitis. The affected area suddenly reddens, followed by rapid progression, with a fever of 39-40℃ developing within several hours. If items 1 to 3, below, are all found, the probability of cellulitis is high:
- 1Redness in the lymphedema region.
- 2The red area feels hot when touched.
- 3High fever (sometimes absent).
It is generally thought that cellulitis develops if bacteria enter a wound. However, in the case of patients with lymphedema, cellulitis develops even without injuries, irrespective of how much care the patient takes. It frequently occurs around the New Year, in early summer, or when patients are particularly busy at work.
If cellulitis occurs repeatedly, it becomes difficult for patients to travel or be involved with their hobbies and interests, etc. In addition, cellulitis may damage the lymphatic vessels and/or make the lymphedema worse. Patients who repeatedly suffer from cellulitis are therefore recommended to undergo appropriate treatment as soon as possible.
Cellulitis treatment
If people who develop cellulitis are able to drink liquid and eat meals, they often recover as a result of treatment at home, without hospitalization. However, if patients find it difficult to drink water due to high fever, or have a continuous high fever, it is often better for them to be hospitalized. Please consult the internal medicine and/or dermatology department at an emergency or general hospital, or your cancer primary-care physician, to decide whether this applies to you.
- 1Rest:While you have a fever, you should rest and conserve your energy.
- 2Antibiotics:These should be prescribed for you by the internal medicine or dermatology department.
- 3Cooling:This is an important aspect of treatment. You should cool the part of your body that has turned red. Roll a bag containing ice water backward and forward on the red, swollen area. This should alleviate the redness and swelling. Note that excessive cooling of a single site can lead to frostbite, so the bag must be rolled evenly, and not kept on a single spot. Alternatively, you can put a wet towel in a plastic bag, and place this on the red area.
*Compression therapy:Edema may be more severe than usual when cellulitis is present, and the usual compression stockings and sleeves may therefore not be appropriate. Pain also sometimes occurs due to inflammation. In such cases, compression therapy can be temporarily suspended. When the pain abates, alleviation of edema can be achieved by starting compression therapy again. However, compression stockings and sleeves can easily cut or work their way into the flesh, and more care than usual is therefore necessary.
*Massages:When redness is present, massages should be avoided.
Cellulitis prevention
- 1Compression therapy should be reconsidered.
- 2Surgery:Lymphatic venous anastomosis
- 3Surgery:Genital lymphatic vesicle resection (if genital lymphatic vesicles are present)
- 4Long-term, oral antibiotic administration
If the appropriate compression therapy is provided, involving elastic stockings, bandages, etc., cellulitis often does not develop. However, if you are currently not confident about undergoing compression therapy, you feel that compression therapy is not sufficiently effective, and/or a mark remains after pressing the affected area with a finger, you should consult a physician whose specialty is lymphedema. If you reconsider compression therapy, it is sometimes possible to alleviate edema, and to hinder the onset of cellulitis. If there are no physicians who can provide the appropriate treatment in your country, you can be treated at our clinic. We will make the appropriate diagnosis, and then present you with a treatment proposal.
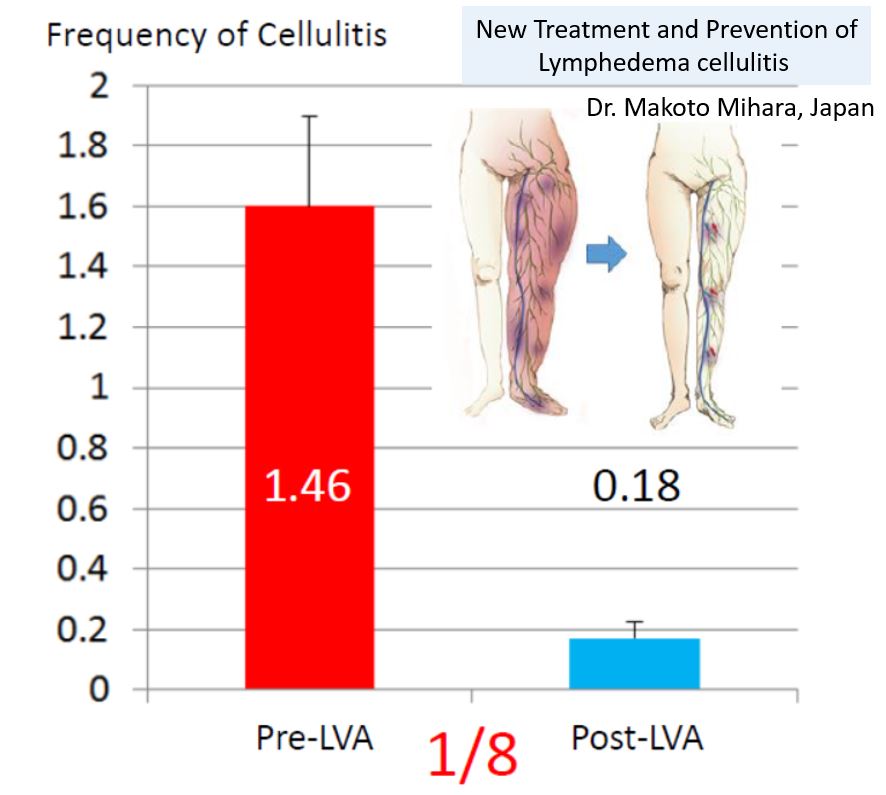
If cellulitis develops despite conservative therapy, surgery is recommended. Lymphatic venous anastomosis reduces the cellulitis rate to about one-eighth. In addition, even if cellulitis develops after this surgery, it is unusual for the fever to reach as high as 38-40℃, often remaining at about 37℃. If the patient rests well, sleeping through the night, symptoms are often markedly reduced the next morning, allowing the patient to carry out the activities of daily life.
The only prophylactic measures for cellulitis in use until now were physiotherapy and long-term oral antibiotic administration, but surgery has recently been accepted as an alternative. Please feel free to consult us or to ask questions about surgery, even if the issues seem small or unimportant.
If you have lymphatic vesicles in the genital region, bacteria can enter your body there, resulting in cellulitis. Treatment of lymphatic vesicles thus prevents the onset of cellulitis.
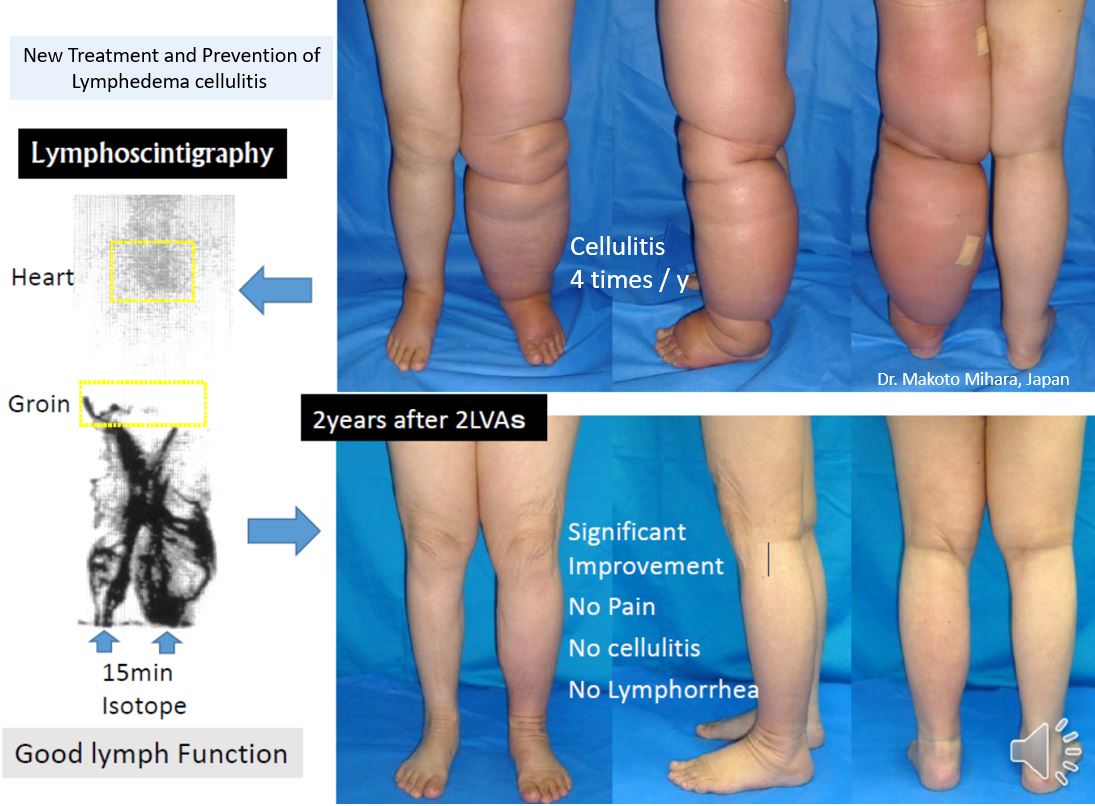
The most important issue is your current lymphatic function, and it is best for you first to undergo an examination by lymph scintigraphy.
Case study of a typical patient with lymphedema-complicating cellulitis
Numerous patients visit our clinic for treatment of lymphedema-complicating cellulitis by our medical team. If lymph scintigraphy confirms that there is residual lymphatic function, and it is judged that lymphatic venous anastomosis (LVA) is indicated, then surgery is recommended. This surgery has been shown to reduce the cellulitis rate in at least 95% of patients.
Our medical team previously treated a patient who arrived at the hospital complaining of the development of cellulitis as often as 20 times a year, but lymphatic venous anastomosis was performed twice, resulting in recovery, without even approximately one occurrence of cellulitis per year. The patient’s long-term postoperative outcome has been stable.
Treatment in Japan
If you have been given the appropriate conservative treatment in your own country, it will take about two weeks from your arrival in Japan to your return to your own country. This time includes diagnosis, and treatment (lymphatic venous anastomosis). If, on the other hand, you have not been given the appropriate conservative treatment in your own country, both conservative treatment and an LVA will be carried out here, and your estimated stay in Japan will be about four weeks.
The surgery itself will be carried out under local anesthetic. There have to date been no cases of postoperative complications such as irreversible nerve damage or bleeding. The annual rate of minor complications, such as lymphatic leakage from the affected area, is less than 1%. In the case of lymphatic leakage, full recovery is achieved gradually by a disinfectant treatment lasting about two weeks.
Before performing an LVA, our medical team will use lymph scintigraphy, indocyanine green lymphangiography, and/or ultrasonography to correctly identify the lymphatic vessel and vein to be operated on. Indocyanine green lymphangiography cannot be carried out with patients who are allergic to CT contrast agents, but the collecting lymphatic vessel can be identified correctly using ultrasonography for such patients. Due to the progress that has been made in these preoperative tests, the results of 10 conventional LVAs are comparable to those of 3 current LVAs, so it is now possible to provide treatment with higher success rates. We currently carry out LVAs on at least 400 limbs per year, which is the largest number for any clinic on the world.
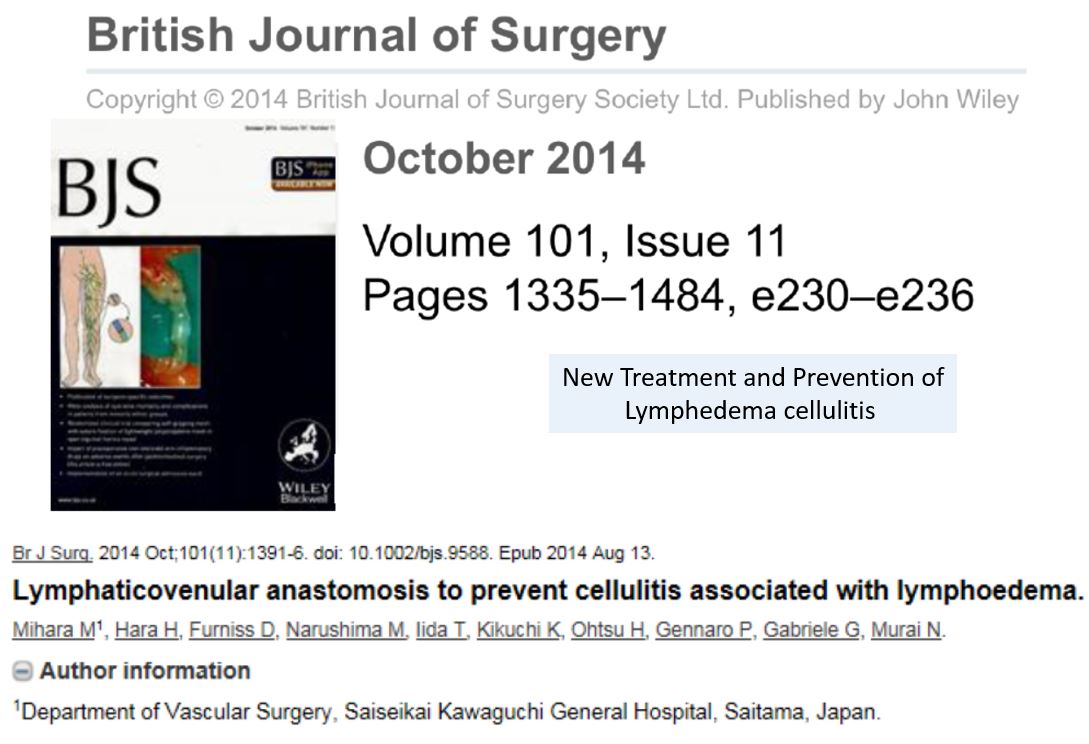
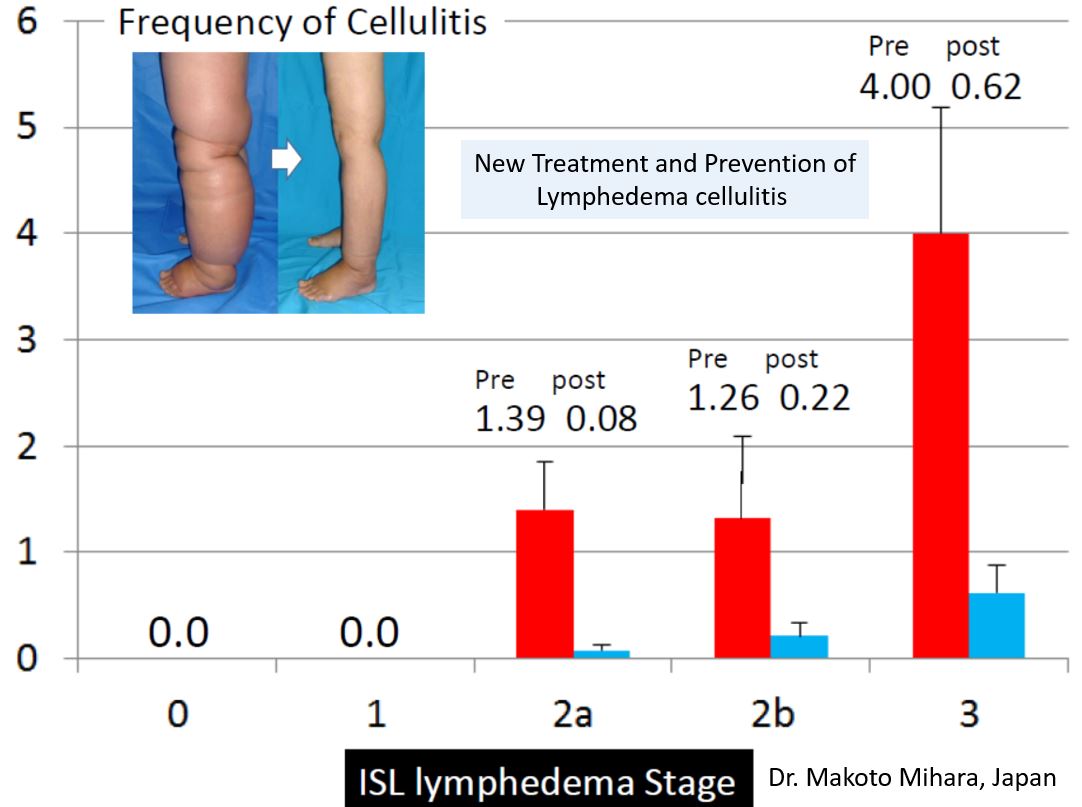
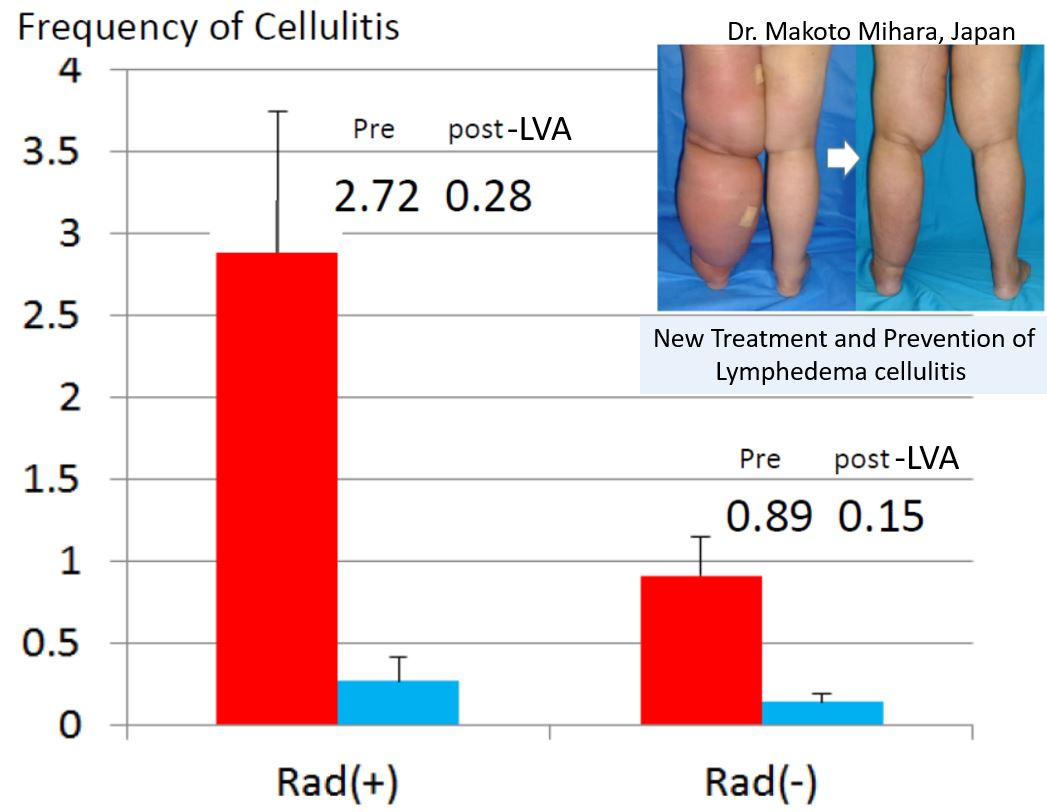
Sicentific data about prevention cellulitis, 2024
In January 2024, our clinic reported new scientific evidence on the prevention of cellulitis in the British Journal of Surgery. We found that the combination of LVA surgery and conservative treatment was more effective at preventing cellulitis than conservative treatment alone. Click here for details of the paper.

Message from Dr. Makoto Mihara
It is now possible to inhibit lymphedema-complicating cellulitis using lymphatic venous anastomosis. Rather than suffering from cellulitis, which can ruin your life, you can instead undergo treatment that has a sound basis in scientific data, thus preventing cellulitis, so that you can enjoy the rest of your life.
We have established medical treatment facilities enabling patients from anywhere on earth to undergo assessment and diagnosis without difficulty, and then to undergo surgery without anxiety. Please feel free to ask us about these.
If any family physician or lymphatic therapist who is responsible for treatment would like to make a surgical study visit, we hold training courses; please feel free to make preliminary consultations in this respect. Physicians and therapists stay one week for such courses, and observe four to seven lymphatic venous anastomosis operations. We also recommend that family physicians and lymphatic therapists visit our clinic together with their patients.
Scientific basis for this treatment
In 2014, we published a report in an international medical journal about reducing the cellulitis rate using lymphatic venous anastomosis. The details are presented below.